Facts to Know Before Beginning a Career in Medical Billing and Coding
Thinking about a career in the healthcare industry but not sure about being involved with direct patient care? Consider choosing training and certification to become a medical coder or medical biller. Healthcare careers under the umbrella of Medical Record Specialists and Health Information Technology include medical billing and coding professionals. Although these two areas of healthcare are not on the front lines of patient care, they are a critical part of a hospital, clinic, or physician’s office practice, especially relating to financial and health insurance matters.
What is Medical Billing and Coding?
A medical coder’s responsibilities include assigning Current Procedural Terminology (CPT) codes and the Healthcare Common Procedure Coding System (HCPCS) which are number and letter codes for a patient’s medical diagnosis, procedure, tests, or interventions done by a healthcare provider. The American Medical Association CPT editorial panel routinely provides ongoing updates, revisions, and changes to CPT codes.
Medical coding is used worldwide, and most countries use the International Classification of Diseases (ICD) coding. ICD is updated by the World Health Organization (WHO) and is modified by each country that is a member of WHO. ICD-11, the latest revision, came into effect in January 2022.
These codes are then used by the medical biller who is responsible for submitting a bill or claim to the patient’s insurance company. This helps determine the appropriate charges for the patient. Medical billers are responsible for communicating with patients about payment and collecting payments for the provider institution or practice.
Every medical procedure, test, or intervention has a specific code used by insurance companies that corresponds with how much insurance companies will pay out in reimbursements to the physician’s office or clinic.
The documentation done by the medical coder and medical biller is needed not only for reimbursement purposes but also to ensure the quality of care for patients. According to the American Academy of Professional Coders, “The medical billing process can be broken down into stages, what’s known as front-end and back-end. Front-end billing takes place pre-service — or before the patient sees the doctor. Back-end billing occurs after the provider sees the patient. Once the medical coder completes their responsibilities and the billing staff have access to the medical codes that represent the patient encounter, the billing process resumes in the back office, which simply means that back-end activities are not patient-facing.”
Career Outlook
The Bureau of Labor and Statistics reports that the medical billing and coding field is expected to grow by seven percent from 2021 to 2031. About 14,900 openings are projected each year, on average, over the decade.
Salaries for medical coders and medical billers can be high-paying. The Occupational Outlook Handbook cites that those working in a medical billing and coding career earned up to $73,370 annually, with the middle 50% earning as high as $44,090. Of course, salaries vary by region and practice.
Certifications
There are several certifications for medical coding and billing that will help you in your career and job search.
Certified Coding Associate (CCA) means that you have basic knowledge of medical coding and billing.
Certified Medical Reimbursement Specialists (CMRS) have skills in facilitating the claims-paying process from the time a service is rendered by a healthcare provider until the balance is paid.
Certified Professional Biller (CPB) enables you to work in inpatient or outpatient settings including long-term care facilities, surgical centers, and dental offices as well as billing companies.
Specialty Certifications
Specialty certifications are also available and mean that the person has expertise in a specialty healthcare setting area. Some of these include Certified Risk Adjustment Coder, Certified Outpatient Coder, Certified Inpatient Coder, Certified Physician Practice Manager, and others.
Blackstone’s online Medical Billing and Coding Program & Career Training prepares students for taking the Certified Coding Associate (CCA) exam administered by the American Health Information Management Association (AHIMA), Certified Medical Reimbursement Specialist (CMRS) exam from the American Billing Association (AMBA), and the Certified Professional Coder (CPC) exam by the American Academy of Professional Coders (AAPC) when they complete the program.
If you are interested in pursuing training for a career as a medical coder or medical biller, know that most students can complete programs in 8-12 months and many are online programs. Check your schedule and know that these careers are in demand and can be rewarding in many ways.
Entry to Expanding Your Healthcare Career
Choosing a career as a medical coder or biller can be a great way to enter the healthcare field to get an idea of the makeup of healthcare settings and interactions. In addition to learning software technology related to coding, medical billing, and healthcare insurance, you will learn medical terminology, anatomy, and physiology. You will also gain knowledge about medical conditions and treatment, diagnostic tests, and procedures. This training can become a gateway to advance your career if you want to pursue direct caregiving as a patient care assistant, nurse, or other healthcare professional.
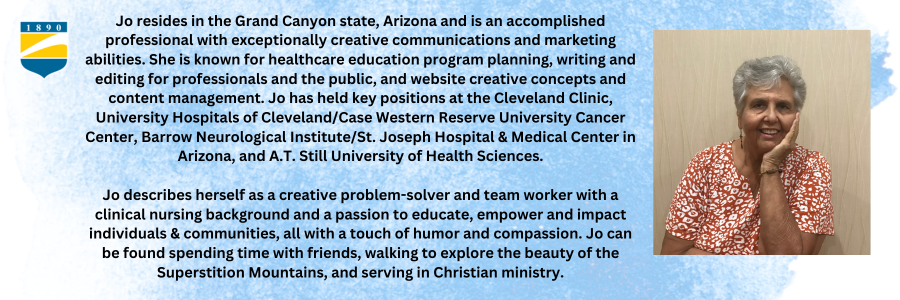
Written by Jo Gambosi